Hope and Healing: Navigating Chronic Pancreatitis Treatment
Chronic pancreatitis is a challenging, long-term condition characterized by persistent inflammation of the pancreas. Unlike acute pancreatitis, which is a sudden inflammation, chronic pancreatitis involves irreversible damage, scarring, and loss of function of the pancreas over time. This vital organ, tucked behind the stomach, is responsible for producing essential digestive enzymes and hormones like insulin. When it’s chronically inflamed, it can lead to debilitating pain, digestive problems, and serious complications, including diabetes and issues affecting the bile ducts and liver.
Navigating Chronic pancreatitis Treatment requires a comprehensive approach and the expertise of specialized medical professionals. The goal of treatment is to manage pain, address nutritional deficiencies, treat complications, and improve the patient’s quality of life.
Understanding the Roots of Chronic Pancreatitis
Chronic pancreatitis can stem from various factors, with long-term, heavy alcohol consumption being a leading cause in many parts of the world. However, other causes include:
- Smoking: Another significant risk factor that can independently contribute to chronic pancreatitis or worsen existing damage.
- Genetic Mutations: Certain inherited genetic defects can predispose individuals to the condition.
- Autoimmune Disorders: In some cases, the body’s immune system mistakenly attacks the pancreas (autoimmune pancreatitis).
- Duct Obstruction: Blockages in the pancreatic duct (where enzymes flow) or common bile duct (which can be affected by gallstones or strictures) can lead to chronic inflammation. This can sometimes involve complications related to Liver Diseases if the bile ducts are affected.
- Idiopathic: In a significant number of cases, the exact cause remains unknown.
Repeated episodes of acute pancreatitis, regardless of the initial cause, can also eventually lead to chronic damage.
The Burden of Symptoms and Complications
The hallmark symptom of chronic pancreatitis is often persistent or recurring upper abdominal pain, which can radiate to the back. This pain can be severe and significantly impact daily life. As the disease progresses and the pancreas loses its ability to produce digestive enzymes, patients may experience:
- Malabsorption: Difficulty digesting fats and other nutrients, leading to weight loss, diarrhea, and foul-smelling, greasy stools.
- Diabetes: Damage to the insulin-producing cells can result in pancreatic-induced diabetes (Type 3c diabetes), requiring insulin therapy.
- Bile Duct Strictures: Scarring can narrow the bile duct, leading to jaundice (yellowing of the skin and eyes) and potentially impacting the liver.
- Pancreatic Pseudocysts: Fluid-filled sacs can form near the pancreas, causing pain or other symptoms.
- Increased Risk of Pancreatic Cancer: Individuals with chronic pancreatitis have a higher risk of developing pancreatic cancer.
The Expert Team for Chronic pancreatitis Treatment
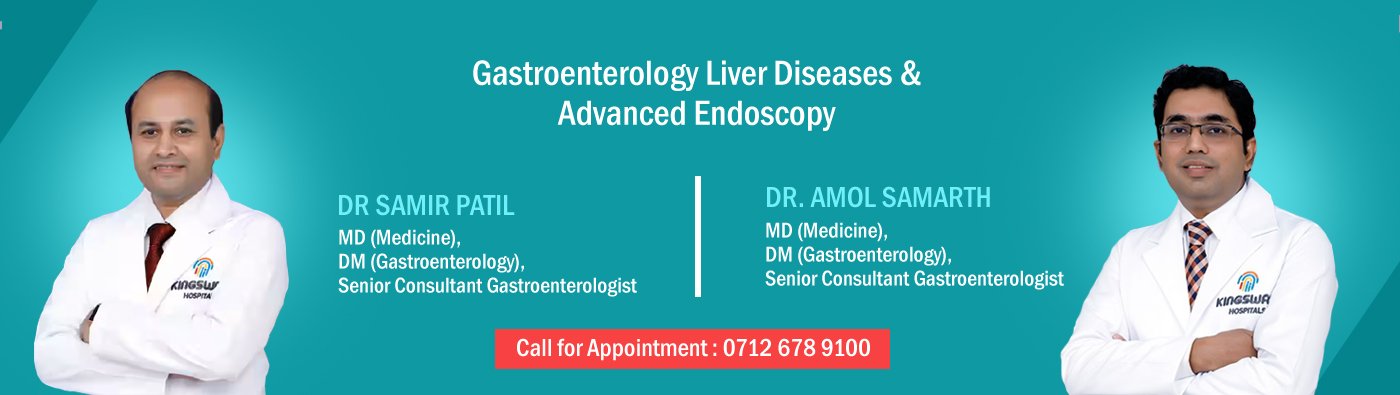
Effective management of chronic pancreatitis is best achieved through a multidisciplinary approach involving specialists experienced in pancreatic disorders:
- Gastroenterologist: These physicians are central to the diagnosis and non-surgical management of chronic pancreatitis. They are experts in digestive health and play a key role in managing pain, prescribing enzyme replacement therapy, and utilizing Endoscopy for diagnosis and treatment of certain complications.
- Hepatologist: If the chronic pancreatitis has led to complications affecting the bile ducts or liver, a Hepatologist, specializing in Liver Diseases, will be an essential part of the care team to manage these specific issues.
- Endoscopy Specialist: A Gastroenterologist with advanced training in therapeutic Endoscopy procedures is crucial for treating complications like duct stones or strictures using minimally invasive techniques.
These specialists work together to create a personalized Chronic pancreatitis Treatment plan for each patient.
Pillars of Chronic pancreatitis Treatment: A Multi-faceted Approach
Chronic pancreatitis Treatment focuses on several key areas:
- Pain Management: Addressing chronic pain is a top priority. This may involve:
- Medications: Starting with over-the-counter pain relievers and progressing to stronger prescription medications as needed.
- Lifestyle Modifications: Avoiding alcohol and smoking is critical, as these can worsen pain.
- Endoscopic Therapy: For pain caused by blockages in the pancreatic duct, Endoscopy can be used to remove stones or place stents to improve drainage.
- Nerve Blocks: In some cases, injections to block nerves that transmit pain signals from the pancreas can provide relief.
- Surgery: For severe, intractable pain not responding to other treatments, surgical options may be considered to decompress the pancreatic duct or remove damaged portions of the pancreas.
Managing Malabsorption: Pancreatic enzyme replacement therapy (PERT) is essential when the pancreas doesn’t produce enough digestive enzymes. Taking these enzymes with meals helps the body properly digest food and absorb nutrients, reducing symptoms like diarrhea and weight loss. Nutritional support and dietary adjustments (often a low-fat diet) are also crucial.
Treating Complications: Endoscopy plays a significant role in managing many complications of chronic pancreatitis:
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This specialized Endoscopy procedure allows for visualization and treatment of issues in the bile and pancreatic ducts. It can be used to:
- Remove Pancreatic Duct Stones: Using baskets or balloons, or sometimes breaking them up with lithotripsy (shock waves).
- Insert Stents: To open narrowed pancreatic or bile ducts (strictures) and improve drainage. This is particularly important for biliary strictures which can affect the liver.
- Drain Pseudocysts: By creating a connection between the cyst and the stomach or small intestine.
Managing Diabetes: If chronic pancreatitis leads to diabetes, it requires careful management with diet, exercise, and often insulin therapy. This is frequently managed by an endocrinologist in coordination with the gastroenterology team.
Lifestyle is Key
Beyond medical and procedural interventions, lifestyle changes are fundamental to managing chronic pancreatitis and preventing its progression. Complete abstinence from alcohol and smoking is paramount. Following dietary recommendations, often involving smaller, more frequent, low-fat meals, can help reduce pain and improve digestion.
Living with chronic pancreatitis can be challenging, impacting physical and emotional well-being. Access to support groups, pain management specialists, and psychological support can be valuable components of Chronic pancreatitis Treatment.
Chronic pancreatitis Treatment is a complex but manageable journey. With the expertise of a skilled team including Gastroenterologists, Hepatologists, and Endoscopy Specialists, leveraging advanced techniques like Endoscopy, and a strong commitment to lifestyle modifications, individuals with chronic pancreatitis can find effective strategies to manage their symptoms, prevent complications like those affecting the Liver Diseases, and live a better quality of life.